Product Usage: This product is intended solely for use as a research chemical. It is designated exclusively for in vitro research and laboratory testing. All information provided on this site is for educational purposes only. It is strictly prohibited to administer this product to humans or animals. Only licensed and qualified professionals should handle it. This product is not classified as a drug, food, or cosmetic and must not be misrepresented or used as such. This product is for research use only. Not for human consumption.
Thymosin Alpha-1
Thymosin alpha-1 is an endogenous peptide that helps coordinate and enhance the activity of the immune system. Since it was first identified in 1972, when researchers purified it from thymus gland tissue, it has been investigated as an immune-modulating agent in a range of conditions, including cystic fibrosis, respiratory diseases, chronic hepatitis, various infections such as tuberculosis and cytomegalovirus, and certain cancers.
Price range: $65.00 through $95.00
All Products
- DESCRIPTION
- STORAGE
What Is Thymosin Alpha-1?
Thymosin alpha-1 is a naturally occurring peptide fragment that was first isolated from thymus tissue in 1972. Since its discovery, it has been investigated in clinical studies for conditions such as cystic fibrosis, a variety of infections (including tuberculosis and cytomegalovirus), respiratory disorders, chronic hepatitis, and several forms of cancer. Thymosin alpha-1 is currently approved in a number of countries for use as an immune-modulating therapy in chronic hepatitis B and C.
Thymosin Alpha-1 Structure
Sequence: Ser-Asp-Ala-Ala-Val-Asp-Thr-Ser-Ser-Glu-Ile-Thr-Thr-Lys-Asp-Leu-Lys-Glu-Lys-Lys-Glu-Val-Val-Glu-Glu-Ala-Glu-Asn
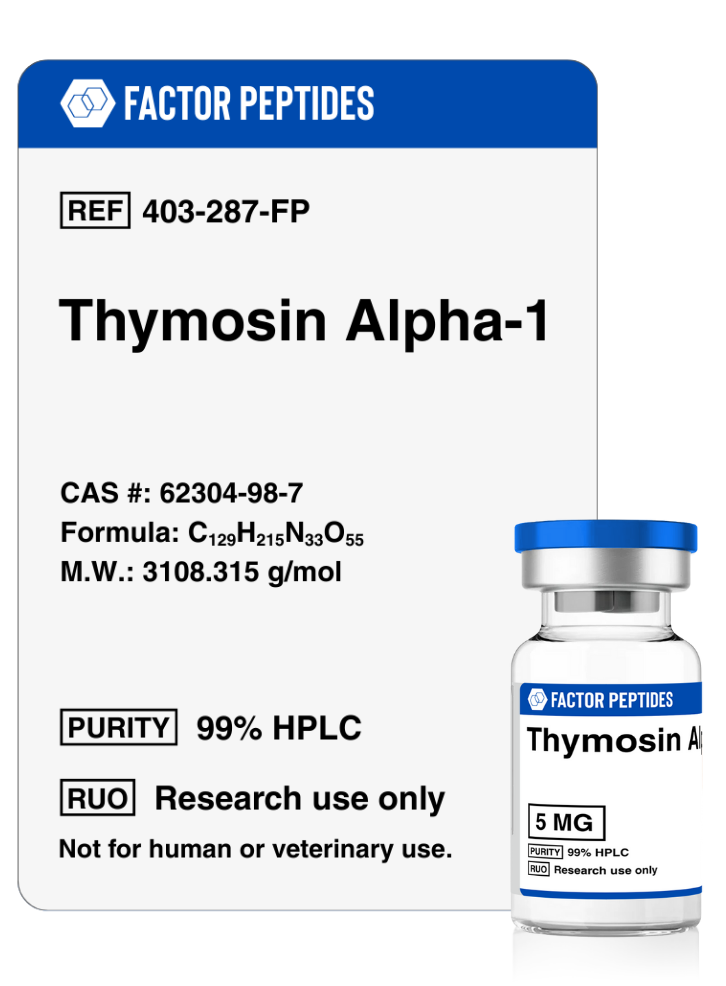
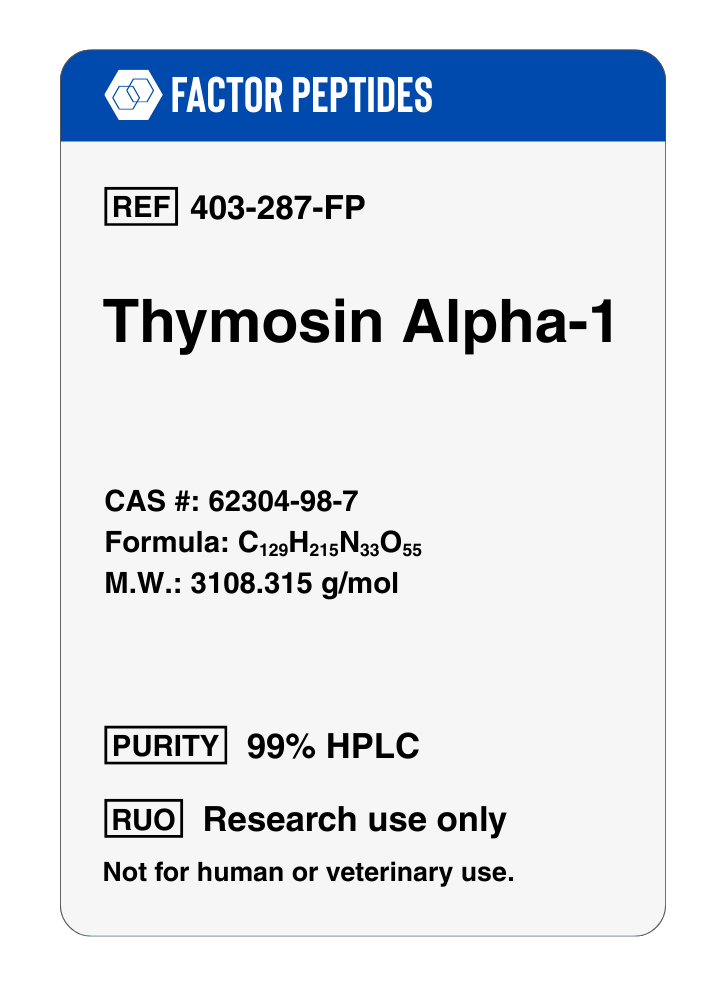
Molecular Formula: C129H215N33O55
Molecular Weight: 3108.315 g/mol
PubChem CID: 16130571
CAS Number: 62304-98-7
Synonyms: Thymalfasin
Thymosin Alpha-1 Research
Thymosin Alpha-1 Modulates the Immune System
Thymosin alpha-1, originally isolated from the thymus gland, is a potent regulator of immune function. The thymus is responsible for producing and maturing T-cells, which are critical for adaptive immunity, immune memory, and coordination of other immune cell types.
Studies in thymectomized mice (mice without a thymus) show that thymosin alpha-1 alone can help restore immune function and limit widespread infection. The peptide influences fundamental aspects of immune signaling, promoting cytokine production and activating pathways that coordinate the activity of multiple immune cell populations. In this way, thymosin alpha-1 exerts broad, positive effects on immune system performance.
One potential application of these properties is as a vaccine adjuvant. Many current vaccines use inactivated (killed) pathogens to avoid the risks associated with live, attenuated organisms. However, inactivated vaccines often elicit weaker and shorter-lived immunity. Thymosin alpha-1 has been studied for its ability to enhance immune responses to inactivated vaccines, with the goal of increasing both the magnitude and duration of protection. This strategy may be particularly relevant for high-consequence infections such as avian influenza, HIV, and others.
Thymosin alpha-1 may also help in settings where the immune response becomes dysregulated, such as sepsis. Sepsis is a life-threatening condition driven by an overwhelming and poorly controlled immune reaction to infection. Early clinical work suggests that thymosin alpha-1 can reduce mortality and lower the risk of long-term complications in septic patients, most likely by helping to restore balanced immune regulation. Ongoing studies are evaluating its role as an adjunctive therapy in sepsis management.
Thymosin Alpha-1 Promotes Nerve Growth
The immune system plays important roles in the growth, development, and maintenance of the central nervous system, especially during early life. Research in mouse models indicates that thymosin alpha-1 can act as a facilitator of neurodevelopment and that peripheral administration may enhance cognitive performance.
The peptide appears to influence the expression of genes involved in neuron growth, synapse formation, and structural connectivity. At the same time, thymosin alpha-1 has been observed to dampen inflammatory pathways that can impair neuronal function. Overall, it creates a microenvironment that favors neural growth and resilience. These findings have prompted interest in thymosin alpha-1 as a potential tool for addressing neurodevelopmental delays and supporting brain repair.
Thymosin Alpha-1 Fights Fungus
Dendritic cells, a specialized class of antigen-presenting cells, are essential for recognizing fungal pathogens and initiating appropriate immune responses. Thymosin alpha-1 has been shown to promote dendritic cell maturation, thereby improving antigen presentation and downstream T-cell activation in experimental models.
In mouse models of invasive aspergillus infection, thymosin alpha-1 enhances T-helper cell activity and improves antifungal immune responses. Because of this, it is being explored as an adjuvant to standard antifungal therapies, with the aim of improving efficacy and outcomes in severe fungal disease.
The central role of dendritic cells in capturing, processing, and presenting antigens makes thymosin alpha-1’s effect on these cells particularly significant. By modulating dendritic cell function at barrier sites such as the skin, respiratory tract, and gastrointestinal tract, thymosin alpha-1 influences immune defense at one of its most fundamental checkpoints.
Thymosin Alpha-1 and Hepatitis
Thymosin alpha-1 has been extensively studied as an immunomodulatory peptide in chronic viral hepatitis. In multiple clinical trials, it has shown benefit as part of combination regimens for chronic hepatitis B and C, often enhancing the response to antiviral therapies and improving markers of immune activity. It has also been used as a vaccine adjuvant to improve responses against hepatitis viruses.
Thymosin alpha-1 is currently approved as a treatment for chronic hepatitis B and C in more than 35 countries, typically as part of broader antiviral protocols and under physician supervision.
Thymosin Alpha-1 and HIV
Despite major advances in antiretroviral therapy, full restoration of immune competence in HIV-positive individuals is often incomplete. Additionally, some antiretroviral regimens have been associated with persistent immune activation and functional abnormalities in certain T-cell subsets, particularly cytotoxic CD8 T-cells.
Thymosin alpha-1 has been studied as an adjunct in this setting, with the goal of restoring more balanced immune regulation and reducing chronic inflammation. Experimental data suggest that thymosin alpha-1 can enhance CD8 T-cell function and promote the release of soluble factors that help protect immune cells from HIV infection and may limit the reactivation of latent virus. These findings support further investigation in combination with standard antiretroviral therapy.
Thymosin Alpha-1 Research and Blood Pressure
Recent research indicates that thymosin alpha-1 can inhibit angiotensin-converting enzyme (ACE), a central component of the renin–angiotensin system involved in controlling blood pressure and vascular tone. Pharmacologic ACE inhibition is a standard strategy for managing hypertension and protecting the heart and kidneys, but many current ACE inhibitors are associated with side effects such as cough and, in some cases, more serious reactions.
By modulating ACE activity, thymosin alpha-1 has been shown experimentally to lower blood pressure and may reduce cardiac remodeling, slow the progression of atherosclerosis, and support kidney function. While these findings are still early and primarily preclinical, they suggest that thymosin alpha-1 or related analogues could one day complement or refine existing ACE-targeted therapies.
Thymosin Alpha-1 Research and Cancer
In vitro studies using human lung cancer cells (A549) indicate that thymosin alpha-1 can exert anti-proliferative effects, reducing both cell growth and metastatic potential. The peptide has also been observed to decrease cell migration, which may help limit local invasion into surrounding tissues.
Clinical and preclinical work combining thymosin alpha-1 with chemotherapeutic agents such as dacarbazine has shown increased progression-free survival without significant additional toxicity, suggesting a possible chemo-sensitizing or immune-supporting role. In animal models, modified long-acting forms of thymosin alpha-1 have demonstrated enhanced efficacy against breast cancer, with increases in CD4 and CD8 T-cell counts and elevated levels of cytokines such as interferon-gamma and interleukin-2.
Thymosin alpha-1 has been or is being investigated as an adjuvant or supportive therapy in multiple malignancies, including:
- breast cancer,
- melanoma,
- hepatocellular (liver) carcinoma,
- lung cancer, and
- colon cancer.
Thymosin Alpha-1 Research and Inflammatory Pain
Inflammatory pain is driven by specific molecular pathways in both the peripheral and central nervous systems. Given the strong anti-inflammatory actions of thymosin alpha-1, researchers have explored its effects on pain signaling.
In mouse models, thymosin alpha-1 has been shown to reduce inflammatory pain by acting directly at sites of inflammation. It lowers the production of pro-inflammatory cytokines and mediators such as TNF-alpha and IL-1beta, which are key drivers of nociceptive signaling. This mechanism is different from that of standard nonsteroidal anti-inflammatory drugs and may, in principle, offer a path to novel analgesic approaches with a distinct side-effect profile.
Thymosin Alpha-1 and Cystic Fibrosis
Cystic fibrosis (CF) is characterized by chronic inflammation, impaired mucus clearance, and recurrent infection, largely driven by misfolding and dysfunction of the CFTR protein. Research has suggested that thymosin alpha-1 can reduce inflammatory signaling and may help improve CFTR function in cellular and animal models.
By combining direct modulation of inflammation with potential improvements in CFTR trafficking or stability, thymosin alpha-1 is being explored as a candidate for integrated, single-molecule approaches to CF therapy, although this work is still at an early stage.
Damaged Teeth and Thymosin Alpha-1
Preclinical studies on avulsed (knocked out) and replanted permanent teeth suggest that thymosin alpha-1 can support better healing of gingival and periodontal tissues and improve the survival of replanted teeth. In experimental models, the peptide appears to enhance soft tissue repair and modulate local immune responses in ways that favor tooth retention following traumatic injury.
The Future of Thymosin Alpha-1
The range of potential applications for thymosin alpha-1 spans viral infection, immune modulation, oncology, neurology, and tissue repair. Notably, the peptide is already in clinical use in several countries as part of approved treatment protocols, particularly in chronic viral hepatitis.
Ongoing work is focused on improving manufacturing efficiency, optimizing dosing strategies, and developing long-acting or modified analogues. There is strong interest in further clinical trials to explore thymosin alpha-1–based approaches for cancer, chronic infection, immune dysregulation, and inflammatory disorders. As an endogenous peptide with a well-characterized safety profile in clinical settings, thymosin alpha-1 continues to attract attention as a versatile immune modulator and research tool.
Thymosin Alpha-1 exhibits minimal side effects and demonstrates low oral and excellent subcutaneous bioavailability in mice. Dose levels used in animal models do not scale directly to humans. Thymosin Alpha-1 for sale at Peptide Sciences is supplied strictly for educational and scientific research only, and is not intended for human consumption or therapeutic use. Only licensed and qualified researchers should purchase Thymosin Alpha-1.
Factor Peptides Storage Guidelines:
These peptides arrive in a dried, stabilized form produced by a process called lyophilization, or freeze drying. In this state, they are generally suitable for transport and short-term storage at typical room temperatures for several months.
Once the dry powder is mixed with bacteriostatic water and turned into a liquid solution, the storage requirements change. The reconstituted solution should be kept in a refrigerator to help maintain its properties, and is usually considered suitable for use for about 30 days under chilled conditions.
Lyophilization involves freezing the material and then exposing it to low pressure so that ice in the sample passes directly from solid to vapor, rather than melting. This leaves behind a light, porous, white solid that is more stable than the original liquid. In this form, the product can often be kept at room temperature until it is time to add diluent.
After delivery, it is good practice to protect the vials from heat and strong light. If the product will be used in the near future, storing the lyophilized powder or reconstituted solution in a refrigerator at temperatures below about 4°C (39°F) is typically appropriate. The dry form often remains intact at room temperature for a number of weeks, so this may also be acceptable when immediate refrigeration is not available and the intended use is relatively soon.
For storage over longer periods, such as many months or years, much colder conditions are preferred. Placing the vials in a deep freezer, around -80°C (-112°F), is commonly used to help preserve the structure and activity of peptides for extended time frames.